Subscribe & Follow
Advertise your job vacancies
Hypertension, diabetes, stroke: they kill more people than infectious diseases and should get a Global Fund
Noncommunicable diseases such as diabetes, hypertension and cardiovascular conditions account for 41 million deaths each year. That's more than 70% of all deaths globally. Most of these deaths (77%) are in low-income and middle-income countries - including those in Africa.

Source: Pixabay
These conditions are currently more prevalent than infectious diseases. Sixty-seven percent occur before the age of 40. Besides being the leading causes of death worldwide, noncommunicable diseases carry a huge cost to individuals. These also undermine workforce productivity and threaten economic prosperity.
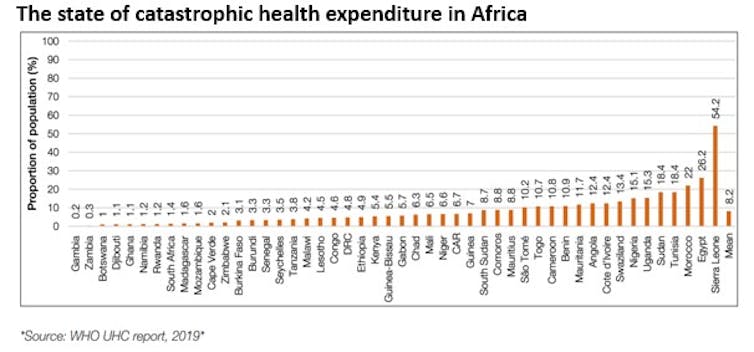
Healthcare provision in much of Africa still relies on external donors. There’s insufficient funding to help low-income and middle-income countries control noncommunicable diseases. Most development assistance for health funding provided by international donors is allocated for infectious diseases and maternal and child health. In 2019, funding for HIV amounted to $9.5bn. The amount allocated to noncommunicable diseases was $0.7bn.
Evidence suggests that addressing the noncommunicable disease pandemic can also mitigate other challenges like HIV, tuberculosis (TB), maternal and child health, and universal health coverage.
The Global Fund to Fight Aids, TB and malaria is an international partnership. The fund invests $4bn a year to fight these three diseases.
I believe it’s now time to think of establishing a Global Fund for noncommunicable diseases, or expand the mandate of Global Fund beyond Aids, TB and malaria. The epidemics of these conditions overlap. For example, research has shown that comorbidities such as diabetes and cancers are common in people living with HIV.
Broadening healthcare provision
Disease-specific programmes have limitations. As public health practitioners we should learn from our mistakes. We must build integrated programmes and health systems that address the interlinkages and co-morbidities. One example would be to include diabetes screening in TB treatment programmes.
In addition to integration, non-communicable diseases require increasing investments.
The Global Fund is seeking $18bn this year. At the same time The Lancet NCD Countdown 2030 projects that interventions for noncommunicable diseases need $18bn a year. That’s what it would take to meet the UN target of reducing noncommunicable diseases by a third by the year 2030.
I would argue that the case for investment in noncommunicable diseases has never been stronger.
A roadmap
The World Health Assembly recently approved the World Health Organization’s roadmap for the prevention and control of noncommunicable diseases covering the period 2023-2030.
The roadmap recommends actions to:
- promote “best-buys” interventions with a high return for every dollar spent, such as smoking cessation programmes
- strengthen health systems
- reduce noncommunicable disease risk factors such as tobacco use and unhealthy diets
- embed noncommunicable diseases within primary healthcare and universal health coverage.
This roadmap needs to be followed in line with the commitments to reduce air pollution and promote mental health and wellbeing.
The lessons learned from the Covid-19 pandemic offer opportunities for strengthening emergency preparedness and responses beyond pandemics. Emergency risk management and continuity of essential health services for all hazards – addressing the foundational health system gaps – can improve health security.
What should be done
How should Africa respond to the increasing burden of noncommunicable diseases? There needs to be a strong political will and buy-in from governments, with strong multi-stakeholder participation.
The UN General Assembly decision on HIV and noncommunicable diseases commits governments to identify and address the comorbidities of HIV and other links to pressing global health challenges. These include links to noncommunicable diseases, learning from the perspectives of people living with these conditions and underscoring the importance of focusing on co-morbidities.
The WHO’s noncommunicable disease compact proposes concrete actions. These actions need to be data-driven and supported by noncommunicable disease-related indicators in health systems performance and access to healthcare metrics.
Monitoring systems need to be more diverse. The systems should capture and monitor progress made through sectors that affect health, such as housing and sanitation. Doing this would strengthen the monitoring of national systems and the capacity to address noncommunicable diseases comprehensively.
Health system strengthening and quality of care will improve significantly with additional resources for noncommunicable diseases through an entity like the Global Fund.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: The Conversation Africa

The Conversation Africa is an independent source of news and views from the academic and research community. Its aim is to promote better understanding of current affairs and complex issues, and allow for a better quality of public discourse and conversation.
Go to: https://theconversation.com/africa
About Kaushik Ramaiya
Kaushik Ramaiya is Honorary General Secretary of Tanzania Diabetes Association which works with Ministry of Health (Tanzania) in implementing National NCD programme which has been funded by World Diabetes Foundation (WDF) and Novo Nordisk Foundation.Related
Almost 50% of adult South Africans are overweight or obese. Poverty and poor nutrition are largely to blame 14 Jun 2024 Biotts makes history: Transdermal insulin delivery 2 May 2024 The rise of Ozempic: how surprise discoveries and lizard venom led to a new class of weight-loss drugs 11 Apr 2024 Man survives pig kidney transplant 8 Apr 2024 Can my dentist diagnose diabetes? 15 Nov 2023 Diabetes is South Africa's second biggest killer disease: hiking the sugar tax would help 6 Nov 2023